Stem cell / bone marrow transplants for children’s cancer

Stem cell transplant replaces diseased or damaged blood cells with cancer-free stem cells.
Diseased or damaged cells can be the result of cancer or cancer treatments (such as high-dose chemotherapy or radiotherapy) where the body’s ability to produce healthy blood cells is affected For example:
- High-risk leukaemia where treatment has failed
- High-dose chemotherapy or radiotherapy given to kill cancer cells can damage bone marrow, so that it doesn’t produce the right amount of healthy blood cells.
- Where the bone marrow is not producing enough healthy blood cells – aplastic anaemia
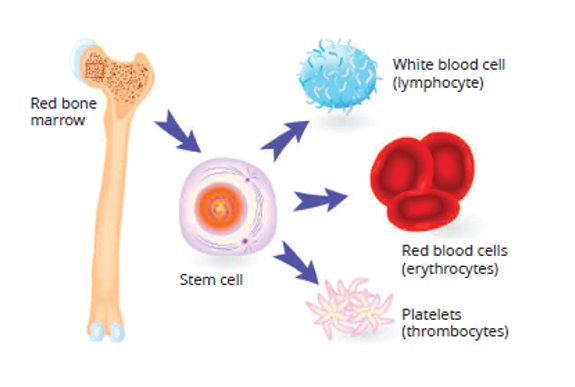
Stem cells are young cells that can grow into different types of blood cells.
The stem cells given in a transplant can grow into new healthy blood cells in your child’s bone marrow.
Types of stem cell transplant
Autologous stem cell transplants
Uses healthy stem cells from your child’s body. The healthy cells are removed before high-dose treatment and then returned to your child. This type of transplant is more likely to be performed for solid tumours and some brain tumours.
How are your child’s stem cells collected?
Stem cells moved from the bone marrow to the bloodstream
This part of the process is called mobilisation. Your child will have daily injections of a drug called G-CSF. This will help your child’s bone marrow to make lots of stem cells. These stem cells then spill out of the bone marrow into the bloodstream.
Your child will have regular blood tests until the amount of stem cells is high enough. Then their stem cells will be collected.
Collecting the stem cells from the blood
You child is attached to a machine called a cell separator. The machine spins and separates the stem cells from the other blood parts. The stem cells are collected into a bag and the remaining blood is then returned to your child. This takes 2-4 hours. Your child can eat and drink normally during the collection. You or a friend may sit with your child during the collection. It’s a good idea to bring your child’s electronic devices, toys, books, music or videos to the unit with them.
Your child may need to have their stem cells collected over 2 or more days to get enough stem cells. The cells will be frozen until needed. If more collections are needed, the growth factor (G‐CSF) injections will be continued.
Possible side-effects
- The medicine (anticoagulant) used to stop the blood clotting in the machine may cause tingling of your child’s lips or the sensation of pins and needles in their fingertips or toes.
- Your child may also experience a funny taste in their mouth and nausea.
- Your child may feel dizzy or light‐headed due to the blood being removed from their body.
You should tell the staff straight away if your child feels any of these symptoms.
Allogeneic (donor) transplant
Uses healthy stem cells from a donor. The healthy cells are given to your child after high-dose treatment. The donor must be a match for your child. The only way to find this out is by doing a blood test called HLA typing. Siblings of your child have a 1 in 4 chance of being a match. If there is no sibling match the hospital will try to find an unrelated donor.
How are donor stem cell transplants done?
Conditioning treatment
Children getting stem cells from a donor will have conditioning therapy to prepare the body for transplant. This conditioning treatment involves high-dose chemotherapy, with or without total body radiation. Conditioning is designed to:
- Suppress the immune system
- Kill cancer cell
- Make space for the stem cells in the bone marrow
Things to know about transplants
- Having a transplant can be hard - physically and emotionally - for both the patient and their family.
- Both types of transplant are long processes.
- With a donor transplant your child will be in hospital for a number of weeks until the donor cells grow and mature into new blood cells. This is called engraftment.
- Side-effects tend to be more severe with high-dose chemotherapy or radiotherapy.
- Because the high-dose treatment destroys your child’s white blood cells, your child will have to be isolated while they recover, as they will be at risk of infection. The length of time depends on the type of treatment and how long it takes for their blood cells to recover. This often takes around 4-6 weeks as an inpatient.
- Most children following transplant will have to be re vaccinated as the treatment can causes them to lose their antibodies that immunise against infection. The transplant team will let you know when it is safe to get your child vaccinated.
If you need support or more information about stem cell transplants, contact the transplant team or you can get in touch with our Children’s Cancer Nurse by calling our Support Line on Freephone 1800 200 700.
For more information
Phone
1800 200 700



