Radiotherapy for children’s cancers
Radiotherapy is a painless treatment using high-energy X-rays that go deep inside the body to kill cancer cells. It may be given:
- To cure
Some treatment protocols may include a course of radiotherapy to shrink a tumour before surgery or to kill any cancer cells that remain after surgery to stop cancer spreading and cure the disease. - To irradiate the whole body (total body irradiation)
This form of radiotherapy is often given to children who are having a bone marrow transplant. - To relieve symptoms (palliative)
Radiotherapy may also be given to relieve symptoms of the disease. Often a short course, sometimes only a single treatment, is needed.
Planning radiotherapy
Radiotherapy must be carefully planned so that the highest dose is given to the tumour area and as little as possible to the nearby cells. As part of the preparation, your child will have a planning CT scan. For younger children, the play specialist can prepare your child in advance.
Marking the radiotherapy area
Marks will be put on your child’s skin to precisely mark the treatment area. It is very important that the marks on the skin are not removed. If the marks fade or disappear, please let the radiotherapy staff know.
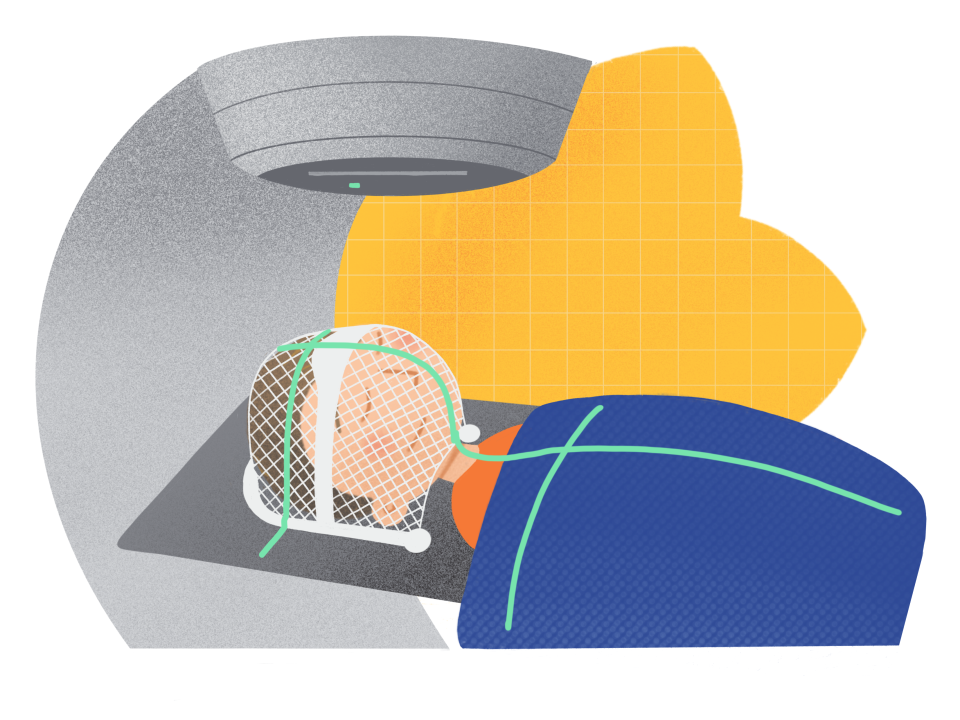
Making moulds
Sometimes your child may wear a plastic mould to make sure that the area to be treated is in exactly the same position for treatment each day. This is usually done for children having radiotherapy to the brain or head and neck region. It is completely painless.
The mould – called an Orfit mould – is made of a soft plastic material, with holes made for the mouth and eyes. After being heated in a warm bath, the plastic changes to the shape of the child’s head and face when it is fitted. The plastic is as flexible as plasticine. If your child is anxious, the family can be in the room when staff are making the mould, as it takes place on the first visit. The Orfit is made on the same day as the planning CT scan is done.
Having radiotherapy
Your child will have his/her radiotherapy at St Luke’s or St James’s Hospital in Dublin.
Having radiotherapy is a bit like having an X-ray. They will lie on a treatment table and the radiotherapy machine will move around them. It doesn’t hurt, but your child might feel nervous or scared while having treatment.
You will not be able to stay in the room with your child during radiotherapy treatment, but you will be able to see your child through a glass window or on a monitor at all times.
The radiotherapy staff are used to dealing with children and can offer great help and support.
Young children
Young children, usually under 3 years of age, will have radiotherapy under a light general anaesthetic.
Older children
Older children may take some time to get used to the size and noise of the machines. But this should get easier once they get to know the staff and their surroundings.
How much radiotherapy will my child need?
Everyone’s treatment is different and individually planned. The dose of radiation your child needs will be decided and divided up into a number of treatment sessions. Treatment could last up to 6 weeks. Radiotherapy is usually given as one session each day for 5 days, with a rest at the weekend.
What are the side-effects of radiotherapy?
Any side-effects tend to affect the area being treated. How severe these side-effects are will vary from person to person, depending on the amount of treatment received. Most side-effects develop during or shortly after treatment and get better within a few weeks. Late side-effects may develop some time after treatment. Some side-effects are long-term or may even be permanent.
Tiredness (fatigue)
Your child may feel very tired during treatment and for a few weeks afterwards. It may take a few months until your child’s energy levels get back to normal.
Nausea and vomiting
Radiotherapy to the brain or the tummy area can cause nausea and vomiting. It can also sometimes lead to loss of appetite and weight loss. Your child's doctor and dietitian can advise and help with this.
Skin reaction in the treated area
The skin the treated area may become red and sore or itchy. The radiotherapy staff will give advice about skin care.
We have information on coping with side-effects.
Other types of radiotherapy
Proton beam therapy
This radiotherapy uses protons instead of X-rays to treat tumours. It does not improve the chance of cure, but it might reduce the risk of long-term side-effects. It is not available in Ireland, but the HSE funds proton therapy in Essen, Germany, for patients that are most likely to benefit from this option. We have a leaflet with more information on proton therapy. You can also ask the Medical Social Worker about charities and groups who may be able to support your family if your child is having this type of treatment.

Coping with radiotherapy
Usually children have radiotherapy every week day with a break at the weekend. For most children there is no need to stay in hospital when they’re having radiotherapy. This means you may need to travel to the hospital every day or stay overnight in Dublin, if you live too far away. This can be tiring and / or expensive.
Help with accommodation and travel
If you live a long way from Dublin it’s best to stay with family or friends in the city or the hospital accommodation, if possible.
If you are travelling to the hospital from your home every day or paying for accommodation, ask the Medical Social Worker about applying for the Travel2Care grant and our Children’s Fund.
- Travel2Care is a fund, made available by the National Cancer Control Programme (NCCP) and managed by the Irish Cancer Society. It is for patients who are having difficulty getting to and from their treatments while attending one of the national centres of excellence.
- Our Children’s Fund is a special fund to help families in financial hardship when their child is faced with a cancer diagnosis. The fund is for families who cannot meet a specific financial burden only because of their child’s cancer diagnosis or treatment. This includes children who are having active treatment or receiving palliative care.
For more information
Phone
1800 200 700



