Surgery for bowel cancer

On this page:
Surgery aims to remove the cancer and the area close to it. Lymph nodes may also be removed to prevent the cancer spreading. Once the tumour is removed, the two healthy ends of your bowel are joined together. This is known as a resection.
You may have a section of your colon or rectum removed, or all your colon or rectum, depending on where the cancer is. For very small cancers you may only need a small procedure which can be done through your mouth or anus.
Types of surgery for colon and rectal cancer
Which part of your bowel will be removed depends on where the cancer is.
- Sigmoid colectomy: removes the sigmoid part of the colon
- Total colectomy: removes all of the colon
- Panproctocolectomy: removes all of the colon and rectum
Ways of doing bowel surgery
Keyhole surgery (laparoscopic surgery)
With keyhole surgery, a small cut is made in your abdomen (tummy area). Your surgeon will put a tube with a tiny telescope and light inside your body through a very small cut. Special instruments can then be used to remove the tumour. There is usually a quicker recovery with keyhole surgery than with open surgery and you may spend less time in hospital . Although the scar on your tummy will be smaller, your bowel will still need the same amount of healing – it’s important you give yourself time to recover.
Your surgeon will discuss if keyhole surgery is suitable for your type of bowel cancer and if this type of surgery is available in your hospital.
Robot-assisted surgery
This is a type of keyhole surgery that uses a computer and robotic arms to help to remove the tumour. Your surgeon will discuss if robot-assisted surgery is suitable for your type of bowel cancer and if this type of surgery is available in your hospital.
Open surgery
A long cut is made in your abdomen. This means your wound will go from below your breastbone down towards your pelvis in a straight line. The length will depend on where the cancer is.
Stomas
Sometimes part of your bowel is brought out onto the surface of your tummy. This is called as stoma. You may have a temporary stoma to allow the join in your bowel to heal. Or some people may have a permanent stoma because it’s not possible to join up the ends of your bowel again. Read more about how to care for your stoma and stoma reversal.
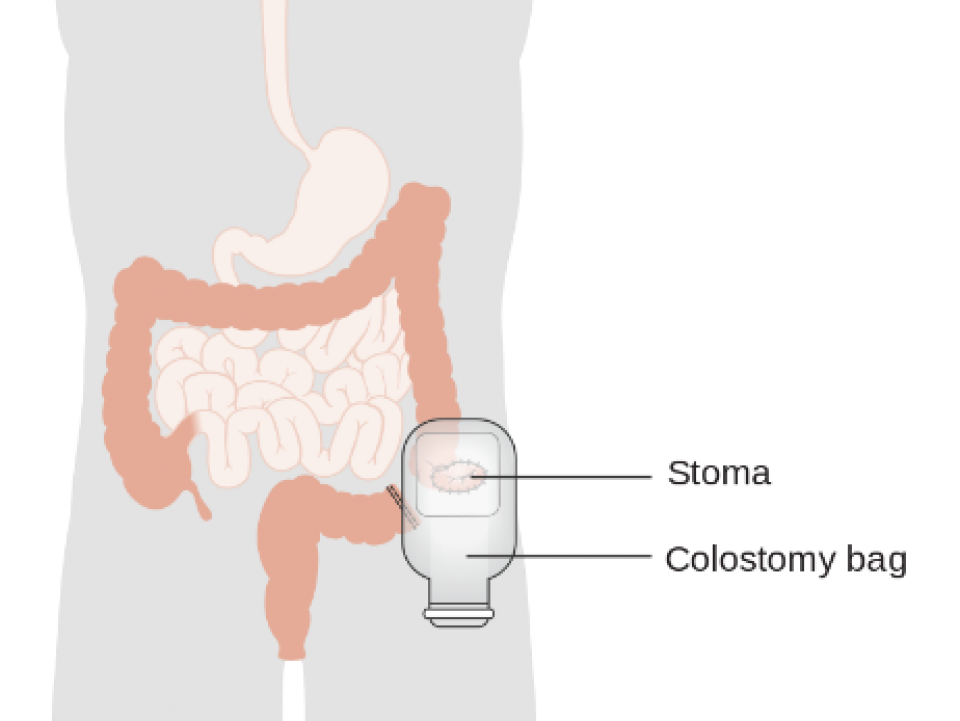
Image courtesy of CRUK/Wikimedia Commons
Will I get side-effects from bowel surgery?
General side-effects: With all surgeries there is a small risk of bleeding and infection. Read more about general side-effects of surgery.
Diarrhoea: Depending on your surgery, you may have diarrhoea for a short while. Drink plenty of clear fluids and let your doctor and nurse know. They can give you medication to control it. If you have an ileostomy, contact your stoma nurse for advice on treating diarrhoea and drinking fluids.
Change in bowel habits: Some people find their bowels are more active after surgery. As a result, you may have to control what you eat for a while. If you have a stoma, your bowels may move at certain times of the day. You may notice that your stoma is more active after a meal or that it works a little bit all day.
Wind (flatulence): Sometimes wind can be a problem. It can build up and give you pain and discomfort. Talk to your nurse about taking peppermint water. Your doctor can prescribe medication to relieve it as well.
Sexual side-effects: While most people have no problem resuming their sex life after bowel surgery, some find it more difficult. Read more about the sexual side-effects of bowel cancer treatments.

Your diet after surgery
At first you may find that some foods affect your bowels or stoma. It may be a few weeks or months before things settle down. Your stoma nurse will advise you about a diet that suits your stoma. It may take some time to find out which foods agree with you and those that do not. For example, too much fibre may cause loose stools or make your bowels more active. Start with light meals and eat them slowly. Avoid big platefuls of food as it can be off-putting. Eating nutritious snacks often can help you to build up to larger portions.
We have more information on eating problems after cancer treatment.
Or you can read our booklet Diet and Cancer. You can get a free copy from a Daffodil Centre or by calling our Support Line on 1800 200 700.
For more information
Phone
1800 200 700




