Treating lung cancer symptoms

Blocked airway
In some cases, cancer in your lung can block your windpipe (trachea) and cause breathing problems, infections or a collapsed lung. The following treatments can help:
Tumour debulking
In some patients, thoracic surgeons can use a number of techniques to remove large amounts of tumour blocking airways to try and improve breathing. This is usually done as part of a treatment approach that would include radiotherapy, to try and prevent the tumour growing back for as long as possible.
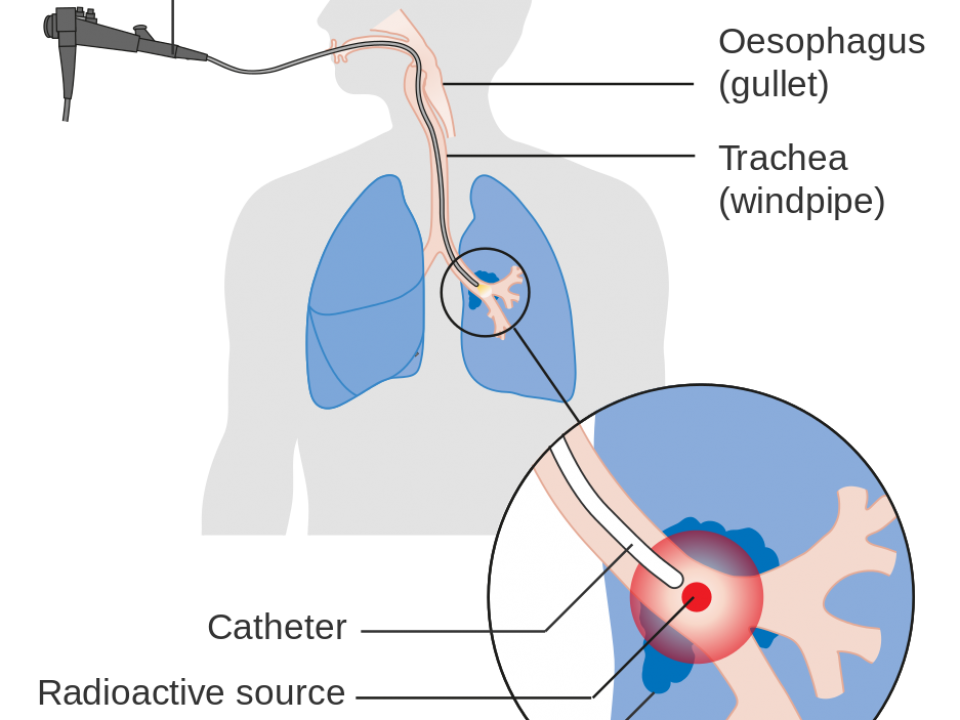
Internal radiotherapy
Sometimes a special type of internal radiotherapy called endobronchial radiotherapy or brachytherapy can help. This is when a source of radiation is put close to or inside the tumour.
Internal radiotherapy may be given if the tumour is blocking one of your airways, causing your lung to collapse, or if you find it hard to breathe.
First, a thin tube called an applicator is put inside your lung for a short while using a bronchoscope. The tube is then linked to another tube that is attached to a machine. When the machine is switched on, it causes the source of radiation to pass inside the tube in your lung. This way of opening up the airway is often done in one session.
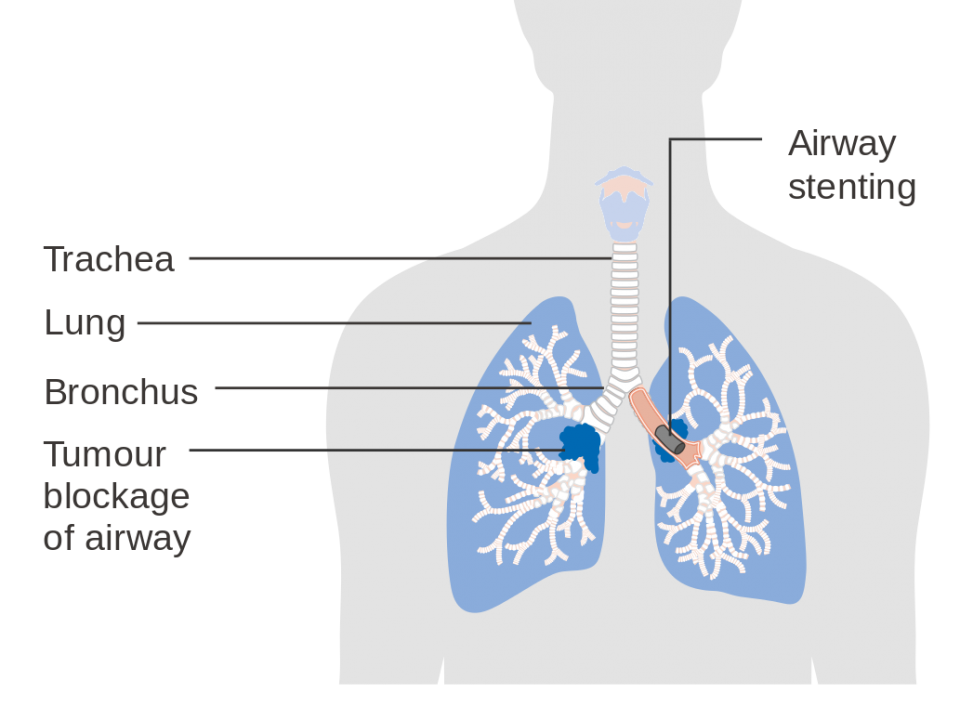
Stenting
Stenting is a treatment that uses a mesh tube, which can hold your airway open and relieve any breathing difficulties caused by the tumour blocking or narrowing your airways.
Stents are usually put in under a general anaesthetic. The stent can stay in your lung permanently if needed. Stents do have a number of side-effects, but they can improve symptoms in some patients.
(Picture courtesy of CRUK / Wikimedia commons)
Cryosurgery
Cryosurgery, or cryotherapy, uses extreme cold to freeze and destroy cancer cells. An instrument called a cryoprobe is placed close to the tumour through a bronchoscope tube. Liquid nitrogen flows through the probe to freeze the tumour. This treatment can be repeated if the tumour grows back.
Chemotherapy, external radiotherapy and ablation treatments may also be used to relieve a blocked airway.
Shortness of breath (dyspnoea)
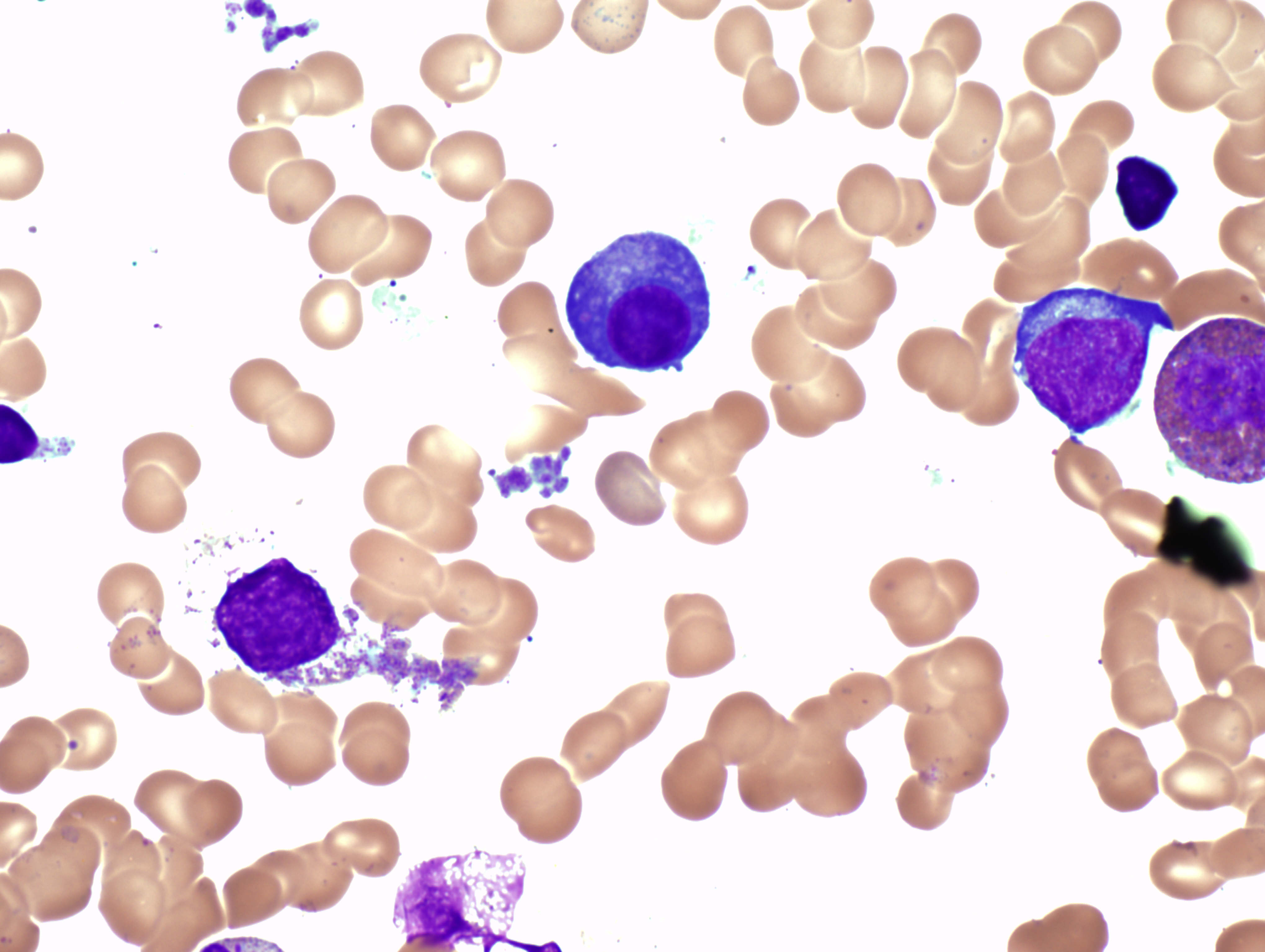
Shortness of breath can be caused by different things. For example, having less lung tissue to give your body oxygen after surgery, fluid on your lungs, a low red blood cell count or a chest infection. The best treatment will depend on what’s causing the problem. Tell your doctor if you are feeling short of breath so that they can find out what’s causing it and recommend the best treatment.
Shortness of breath can be very uncomfortable and distressing. It may be caused by the tumour itself, by increased fluid around your lung or because of treatment.
Discuss this problem with your doctor, GP or nurse. They can decide what to do. It may be possible to relieve the problem that is causing the shortness of breath. For example, if you have extra fluid on your lung, removing this fluid may improve your breathing (see below for details). Another way to relieve the shortness of breath can be through breathing exercises. For example, by using an incentive spirometer.
Other ways of helping to ease shortness of breath could include a blood transfusion if you have a low red blood cell count or medicines such as antibiotics if you have a chest infection, or steroids or water tablets. Your doctor may organise oxygen therapy at home for you if they feel it will help.
Fluid on the lungs (pleural effusion)
Fluid may build up between the linings of your lung. This is known as a pleural effusion and can cause you to feel short of breath.
Your doctor may take a sample of this fluid using a small needle or may decide to drain the fluid. This can be done by putting a small tube into your chest under local anaesthetic. The tube can then be removed once all the fluid has stopped draining.
Shortness of breath will usually improve after the fluid is drained. If the drainage has improved your symptoms and if the fluid starts to build up again, your doctor may decide to do a pleurodesis. Pleurodesis involves putting medication into your lungs to make the linings of your lung stick together. This can prevent fluid building up again. It may be done under local or general anaesthetic.
Cough
An irritating, persistent cough can really affect your quality of life. You may complain of not being able to sleep, shortness of breath and pain. It is important to find out the cause of the cough. The tumour, a chest infection or bronchitis may cause the cough. Treatment with certain medicines, radiotherapy or antibiotics may help.
Tips:
- Drink plenty of fluids, such as water and fruit juice, if you are coughing up a lot of phlegm. This will loosen it and make it easier to cough up.
- Ask your doctor or nurse to recommend a good cough mixture.
- Tell your doctor if your cough is dry and irritating. You may not be coughing up any phlegm. They may give you medicine to reduce or stop the cough.
Avoid situations that make your cough worse, such as a smoky atmosphere or sudden changes in temperature. Make sure you have fresh air wherever you are sitting. Open a window or use a fan to create a light breeze.
Pain
A lung tumour can cause mild to severe pain in your chest by pressing on nearby tissues and organs. Pain can also be caused by the tumour spreading to other parts of your body, such as your bones. The pain may be constant or present only now and then.
Your doctor will try to find out what is causing the pain. Surgery, radiotherapy and chemotherapy can all help to ease pain. Your doctor will decide which painkiller is best suited to the type of pain you have. If the medication does not control the pain, tell your doctor or nurse.
A specialist who manages pain and other symptoms may also be able to help you. They can arrange for you to try out different painkillers to find out what suits you best. There are also other ways to treat pain, such as nerve blocks and epidural injections. If you need more information, ask your doctor or nurse. You may be referred to the palliative care team who are experts in managing symptoms, including pain.
Read more about managing pain.
Fatigue
Fatigue is a common symptom of cancer, often described as an overwhelming tiredness. Fatigue can carry on for some time, even after treatment has ended.
Tell your doctor if fatigue is bothering you, so they can find the cause and give you advice and treatment to help.
For more information
Phone
1800 200 700